Nursing interventions for migraine headaches offer a multifaceted approach to managing this debilitating condition. This comprehensive guide delves into the pathophysiology, assessment, non-pharmacological and pharmacological interventions, patient education, and evidence-based practice surrounding migraine headaches, empowering nurses with the knowledge and skills to provide optimal care.
The intricate interplay of genetics, environmental triggers, and neurovascular changes underscores the complex nature of migraine headaches. Nurses play a pivotal role in assessing patients, employing a range of techniques to establish a precise diagnosis and guide appropriate treatment plans.
Pathophysiology of Migraine Headaches
Migraine headaches are a common neurological disorder characterized by severe, throbbing pain in the head. The exact pathophysiology of migraine headaches is not fully understood, but several mechanisms are thought to be involved.
One theory suggests that migraines are caused by a disturbance in the trigeminovascular system, a network of nerves that supply the head and face. When activated, this system releases inflammatory mediators, such as calcitonin gene-related peptide (CGRP), which can cause blood vessels in the head to dilate and become inflamed, leading to pain.
Another theory implicates genetics in the development of migraines. Studies have shown that migraine headaches tend to run in families, suggesting that certain genes may increase a person’s susceptibility to the condition.
Environmental triggers, such as stress, certain foods, and changes in sleep patterns, can also trigger migraines in some individuals.
Assessment of Migraine Headaches: Nursing Interventions For Migraine Headaches
The diagnosis of migraine headaches is based on a combination of factors, including a detailed medical history, physical examination, and diagnostic criteria.
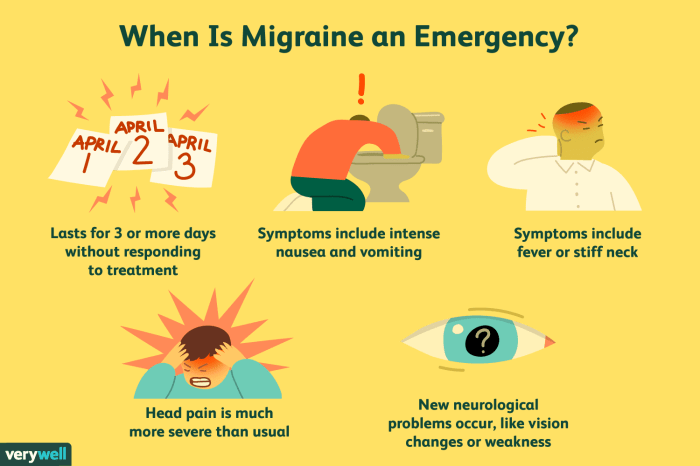
During the medical history, the healthcare provider will ask about the patient’s symptoms, including the location, duration, and severity of the pain, as well as any associated symptoms, such as nausea, vomiting, and sensitivity to light and sound.
The physical examination may include a neurological examination to assess for any neurological deficits. The healthcare provider may also perform a head and neck examination to rule out any other potential causes of the pain.
The International Headache Society (IHS) has established diagnostic criteria for migraine headaches, which include:
- At least five episodes of headache that meet the following criteria:
- Pain is unilateral, pulsating, and of moderate to severe intensity.
- Headache lasts for 4-72 hours (untreated).
- Headache is aggravated by routine physical activity (e.g., walking or climbing stairs).
- Headache is associated with nausea and/or vomiting, and/or photophobia and phonophobia.
Non-Pharmacological Nursing Interventions
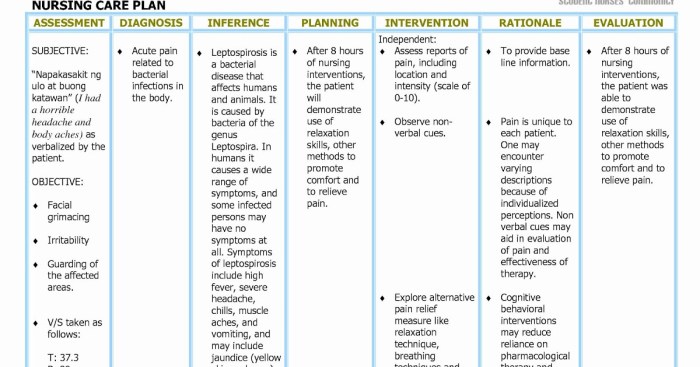
Non-pharmacological nursing interventions for migraine headaches aim to reduce the frequency and severity of attacks and improve the patient’s quality of life.
These interventions may include:
- Relaxation techniques, such as deep breathing, meditation, and yoga
- Stress management strategies, such as cognitive-behavioral therapy and biofeedback
- Lifestyle modifications, such as regular exercise, a healthy diet, and adequate sleep
- Acupuncture
- Massage therapy
- Heat or cold therapy
Pharmacological Nursing Interventions
Pharmacological nursing interventions for migraine headaches involve the use of medications to prevent or treat attacks.
The following table summarizes the different classes of medications used to treat migraine headaches:
| Medication Class | Mechanism of Action | Side Effects | Dosing Regimen |
|---|---|---|---|
| Triptans | Serotonin (5-HT1B/1D) receptor agonists | Nausea, vomiting, dizziness | As needed, up to 4 doses per day |
| Ergotamines | Vasoconstrictors | Nausea, vomiting, diarrhea | As needed, up to 2 doses per day |
| Opioids | Bind to opioid receptors in the central nervous system | Nausea, vomiting, drowsiness | As needed, up to 2 doses per day |
| Anti-emetics | Prevent or treat nausea and vomiting | Drowsiness, dizziness | As needed, up to 4 doses per day |
| NSAIDs | Non-steroidal anti-inflammatory drugs | Gastrointestinal upset, bleeding | As needed, up to 4 doses per day |
Patient Education and Support
Patient education is an essential component of managing migraine headaches. Nurses play a vital role in educating patients about their condition, treatment options, and self-management strategies.
Effective patient education should include the following:
- Information about the pathophysiology of migraine headaches
- Identification of triggers and preventive measures
- Instructions on how to use medications properly
- Strategies for managing stress and anxiety
- Resources for support groups and other resources
Expert Answers
What are the common non-pharmacological interventions for migraine headaches?
Non-pharmacological interventions include relaxation techniques (e.g., deep breathing, meditation), stress management strategies (e.g., biofeedback, cognitive-behavioral therapy), and lifestyle modifications (e.g., regular sleep patterns, avoiding triggers).
How do nurses educate patients about migraine management?
Nurses provide education on migraine triggers, medication use, lifestyle modifications, and self-care strategies. They empower patients to actively participate in their care and make informed decisions.
What are the latest research findings on nursing interventions for migraine headaches?
Research supports the effectiveness of non-pharmacological interventions, such as relaxation techniques and stress management, in reducing migraine frequency and severity. Additionally, studies highlight the importance of patient education and support in improving outcomes.